Introduction:
Afferent Pupil Defect (APD) is a condition that can affect an individual’s vision and how their pupils respond to light. This neurological disorder is typically identified during a routine eye examination and often signals an underlying problem within the optic nerve or visual pathways. Understanding Afferent Pupil Defect is essential for proper diagnosis and treatment, as it can be linked to various neurological disorders. In this article, we will delve into the details of APD, from its causes to how it is diagnosed, the symptoms associated with it, and available treatment options.
1. What is Afferent Pupil Defect?
Afferent Pupil Defect refers to a condition where there is an abnormal response to light in one or both of the pupils. Normally, when light is shined into one eye, the pupil constricts (becomes smaller), and the other pupil constricts as well, even without direct light. This is a normal response of the pupillary light reflex. However, in individuals with APD, the pupil may fail to constrict appropriately when light is shined into the affected eye.
- Normal Pupil Reflex:
When light hits the retina, it sends signals through the optic nerve to the brain. The brain then sends a message back to the eye to constrict the pupil in response to the light. In cases of APD, this reflex is impaired, often due to issues with the optic nerve or the pathways transmitting visual information. - Types of Afferent Pupil Defect:
APD can be classified based on the severity and cause of the defect. A mild APD might result in slight differences in pupil response, while a more severe form can cause noticeable differences in pupil sizes.
2. Causes of Afferent Pupil Defect
The causes of Afferent Pupil Defect are diverse and often related to damage in the optic nerve or visual pathway. Some of the common causes include:
- Optic Nerve Diseases:
Any condition that affects the optic nerve can lead to APD. Examples include optic neuritis, which is often caused by multiple sclerosis, and optic neuropathy, which can occur due to poor blood supply or pressure on the optic nerve. - Retinal Disorders:
Diseases that affect the retina, such as diabetic retinopathy or macular degeneration, may result in APD. These conditions damage the retina’s ability to send visual signals properly. - Glaucoma:
Chronic glaucoma can damage the optic nerve over time, potentially leading to APD. Increased pressure in the eye due to glaucoma is a common culprit in optic nerve damage. - Brain Lesions:
Lesions or tumors affecting the brain’s visual processing areas can also cause Afferent Pupil Defect. Such damage can interrupt the communication between the optic nerve and the brain, leading to abnormal pupil responses. - Trauma or Injury:
Trauma to the eye, optic nerve, or head can disrupt the normal functioning of the pupil reflex.
3. Symptoms of Afferent Pupil Defect
Individuals with Afferent Pupil Defect may not always notice symptoms immediately. However, once detected, the condition can be associated with several signs that are important for diagnosis:
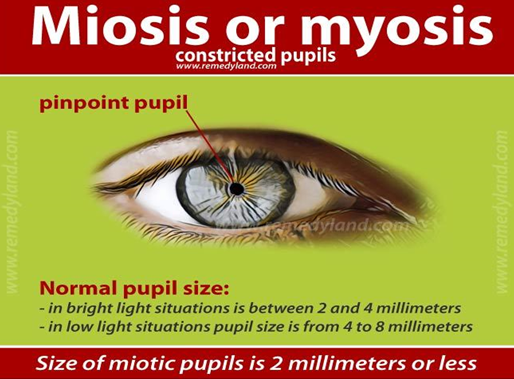
- Abnormal Pupil Response to Light:
The hallmark symptom of APD is an abnormal response of the pupil when exposed to light. The pupil may dilate instead of constricting in response to light. - Unequal Pupil Sizes (Anisocoria):
APD may cause unequal pupil sizes, with one pupil appearing larger than the other, even in normal lighting conditions. This condition can be most noticeable in dim light or when a bright light is shined in the eye. - Reduced Visual Acuity:
In some cases, Afferent Pupil Defect is associated with decreased vision in one or both eyes, especially if the defect is caused by damage to the optic nerve or retina. - Loss of Peripheral Vision:
Depending on the underlying cause of APD, a person may experience a loss of peripheral vision, making it difficult to see objects outside of the central visual field.
4. How is Afferent Pupil Defect Diagnosed?
Diagnosing Afferent Pupil Defect usually begins with a thorough eye examination and a test called the pupillary light reflex. The following methods are commonly used:
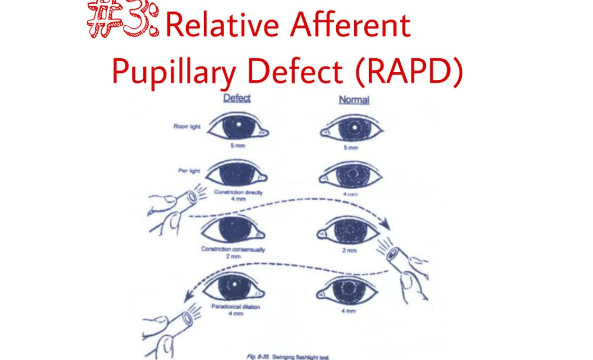
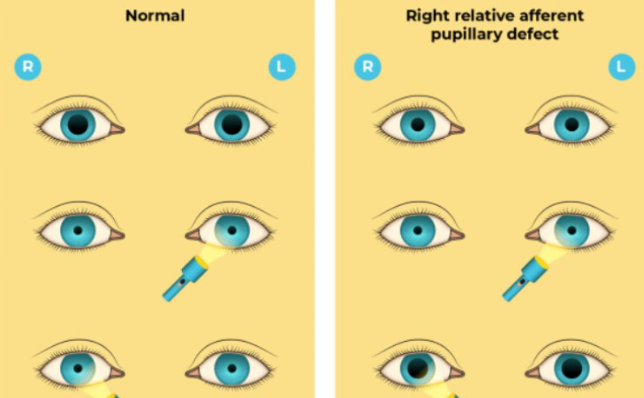
- Swinging Flashlight Test:
This test is one of the most common methods used to diagnose APD. The examiner shines a light into each eye while moving it back and forth between the two eyes. In normal circumstances, both pupils constrict equally. However, if there is an afferent pupil defect, the pupil in the affected eye will fail to constrict properly. - Visual Field Test:
A visual field test may be conducted to assess the range of vision in each eye. This can help identify whether there is any vision loss associated with the condition. - Ophthalmoscopy:
Ophthalmoscopy is used to examine the retina and optic nerve for any abnormalities, such as damage caused by optic neuritis, glaucoma, or retinal disease. - MRI or CT Scans:
In some cases, imaging techniques like MRI or CT scans may be recommended to identify potential lesions or tumors affecting the brain’s visual processing centers or the optic nerve.
5. Treatment and Management of Afferent Pupil Defect
The treatment of Afferent Pupil Defect depends on the underlying cause. In many cases, addressing the root cause can help manage or reduce the symptoms associated with the defect:
- Medications for Underlying Conditions:
For conditions like optic neuritis or multiple sclerosis, corticosteroids and other medications may be prescribed to reduce inflammation and prevent further damage. - Surgical Interventions:
In cases where the APD is caused by a tumor or other physical obstruction, surgery may be required to remove the lesion and relieve pressure on the optic nerve. - Managing Glaucoma:
For individuals with glaucoma, treatments to lower intraocular pressure, such as eye drops or surgical interventions, can help manage the condition and prevent further optic nerve damage. - Vision Rehabilitation:
In some cases, vision rehabilitation may be recommended, including the use of visual aids to assist with daily activities. If the vision loss is significant, low-vision aids can help individuals maintain independence.
6. Frequently Asked Questions about Afferent Pupil Defect
Q1: Can Afferent Pupil Defect cause blindness?
A1: While Afferent Pupil Defect itself does not directly cause blindness, it can be a sign of underlying conditions that may lead to vision loss, such as optic nerve damage or retinal disorders.
Q2: Is APD always noticeable?
A2: No, in some cases, Afferent Pupil Defect may not be immediately noticeable, and it is often detected during routine eye exams or when a person is evaluated for other vision-related issues.
Q3: Can APD be treated completely?
A3: The treatment of APD largely depends on its underlying cause. Some conditions can be managed or treated effectively, while others may not be reversible. Early diagnosis and treatment are key to improving outcomes.
7. Conclusion: Managing Afferent Pupil Defect for Better Vision Health
Afferent Pupil Defect can be an alarming sign of an underlying neurological or ocular condition. However, with timely diagnosis and appropriate treatment, the symptoms can be managed, and in some cases, vision can be preserved. Understanding the causes and treatment options for APD is essential for anyone experiencing visual disturbances or irregular pupil responses. If you suspect you may have Afferent Pupil Defect, consult with a healthcare professional to begin the diagnostic process and determine the best course of action for your eye health.